Medicare can start covering certain weight loss drugs for the first time — as long as they are approved for an added health benefit, the Centers for Medicare and Medicaid Services said Thursday.
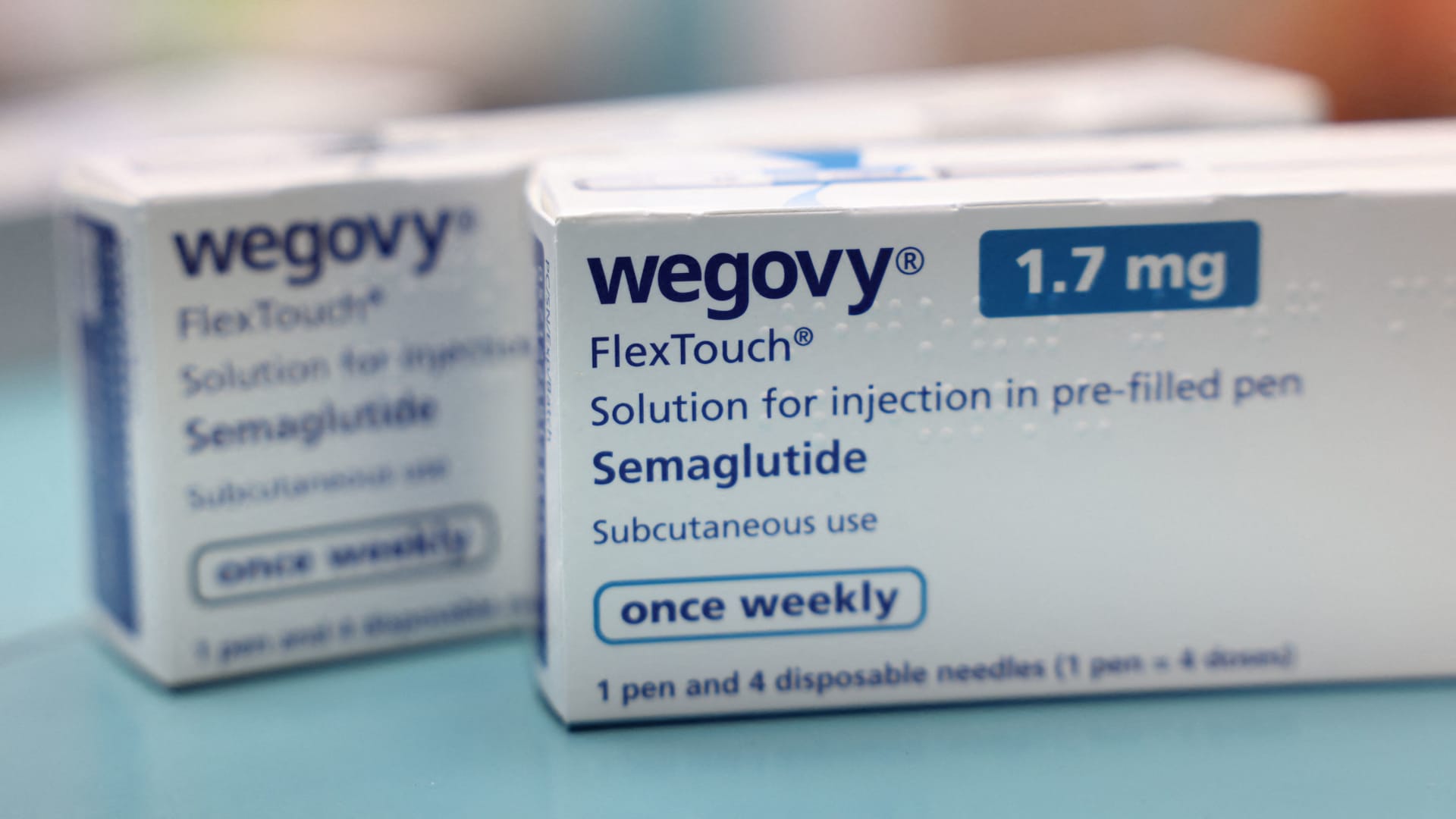
That opens the door for broader coverage of some highly popular weight loss medications such as Novo Nordisk‘s Wegovy, which is now approved in the U.S. for heart health. Those treatments have skyrocketed in demand over the past year despite their hefty price tags and spotty insurance coverage.
Under the new CMS guidance, Medicare Part D plans can cover obesity treatments that receive Food and Drug Administration approval for an additional health benefit. Medicare prescription drug plans administered by private insurers, known as Part D, currently cannot cover those drugs for weight loss alone.
The agency’s guidance means Medicare patients could soon get coverage for Wegovy, as long as they have obesity and a history of heart disease and are prescribed the treatment to reduce their risk of heart attacks and strokes. Earlier this month, the Food and Drug Administration approved Wegovy for that purpose.
The guidance also will open the door to future coverage of other weight loss medications, many of which are being tested for additional health conditions.
Drugmakers such as Novo Nordisk, which also makes the diabetes drug Ozempic, and Eli Lilly are studying their weight loss medicines as treatments for fatty liver disease, chronic kidney disease, sleep apnea and more. To be covered, those drugs would need to return late-stage trial results and then be submitted for FDA approval for those uses.
Wegovy is part of a class of drugs called GLP-1s which mimic a hormone produced in the gut to suppress a person’s appetite and help regulate blood sugar. Coverage for those treatments when used for weight loss is a mixed bag.
Roughly 110 million American adults are living with obesity and approximately 50 million of them have insurance coverage for weight loss drugs, a spokesperson for Novo Nordisk said in a statement last week.
Some of the nation’s largest insurers, such as CVS Health’s Aetna, also cover the treatments.
But many employers don’t. An October survey of more than 200 companies by the International Foundation of Employee Benefit Plans, or IFEBP, found only 27% provided coverage for GLP-1s for weight loss, compared with the 76% that covered those drugs for diabetes. Notably, 13% of employers indicated they were considering coverage for weight loss.
A provision of a 2003 law established that Medicare Part D plans can’t cover drugs used for weight loss, but the program does cover obesity screening, behavioral counseling and bariatric surgery. A group of bipartisan lawmakers have introduced legislation that would eliminate the provision, but its fate in Congress is far from certain.
A CMS spokesperson told CNBC last week that Medicaid programs would be required to cover Wegovy specifically for its new cardiovascular use. By law, Medicaid must cover nearly all FDA-approved medications, but weight loss treatments are among a small group of drugs that can be excluded from coverage. Around 1 in 5 state Medicaid programs currently cover GLP-1 drugs for weight loss.