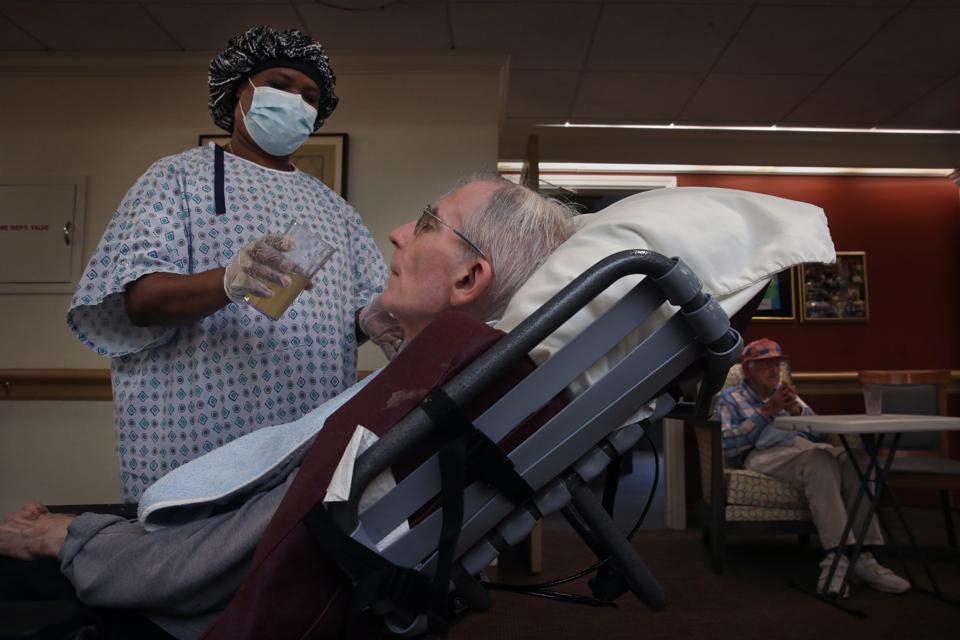
BOSTON, MA – SEPTEMBER 2: A Care partner helps a resident during lunch at an assisted living … [+]
Boston Globe via Getty Images
The statistics simply are staggering. More than 728,000 residents and staff of long-term care facilities have contracted covid-19 over the past nine months. More than 100,000 have died—a number that has doubled since June. That is equal to roughly the entire population of San Mateo CA, or Green Bay WI.
Four of every 10 covid-19 deaths in the US have been residents or staff of nursing homes or assisted living facilities. In 15 states, they account for at least half the deaths.
It is shameful. It is scandalous. And, at least to some degree, it did not have to happen. People died because government and facilities failed to do their jobs. Testing remains costly, slow, and inaccurate. Facilities remain understaffed and some staffs remain poorly trained and badly supervised. State, local, and federal rules are inconsistent and hard to understand.
Government funding of long-term care is insufficient. Nursing home regulators are failing to enforce violations of infection control standards. And millions of people in the broader community won’t take the simple steps necessary to slow the spread of the virus, thus effectively assuring outbreaks among the most vulnerable.
We knew what to do
It is not as if we did not know what to do. For those who cared to pay attention, the early covid-19 experiences in Northeastern states like New York and Connecticut provided a clear roadmap. But we largely ignored those lessons so we repeated many of the same mistakes in the South and Southwest in the summer. And killed more frail older adults
People died because other people won’t wear masks or social distance. Because they go to bars, catch the disease, then spread it to direct care workers who then (often unknowingly) transmit it in the facilities where they work. Because the President of the United States insists a disease that has killed more 270,000 Americans is a hoax and mocks people who wear masks.
MORE FOR YOU
The latest data about covid-19 and long-term care facilities are from the Kaiser Family Foundation and, while they are the most reliable available, they understate the true number of cases and deaths. One state doesn’t report data at all, others are slow to report. Some include assisted living facilities and others do not. And many non-fatal cases probably went unreported, especially in the pandemic’s early days.
Death from social isolation
Finally, these deaths exclude those who may not have passed away directly from covid-19, but who died from the disease’s indirect effects. This especially is true about those residents of long-term care facilities that have been closed to visitors for eight months. Imagine what it is like to be living in a facility and unable to have any personal contact with family members beyond phone calls or facetime. Not so different than prison.
We don’t know how many residents have died from loneliness, but we do know that many are suffering from what is called “failure to thrive” and dying prematurely. Privately, nursing home operators acknowledge that many residents, frequently those with dementia, are suffering from depression and dying sooner than expected.
If the expectations of public health experts are correct, we are about to go on a wild roller-coaster ride for long-term care residents. In the short-term, expect another brutal round of illness and death, due to the widespread travel and socializing among the broader population over Thanksgiving and an expected repeat at the end of this month. We know—and have known for months—that the biggest single driver of covid-19 in long-term care facilities is spread of the virus in the communities where these facilities are located.
The pandemic has exploded across the US over the past month and public health experts expect it to get far worse over the next few weeks. And that will almost surely mean more illness and death in long-term care facilities. Thousands more frail older adults will die.
Vaccines are coming
But just over the horizon are the vaccines. Assuming no unpleasant surprises, the Food and Drug Administration could approve at least two vaccines—produced by Pfizer and Moderna—for distribution within a few days and available to providers within a couple of weeks.
Health-care workers (including, perhaps, nursing home staff) and first responders are likely to be at the head of the line, followed by other essential workers such as teachers and food workers, and then older adults with underlying health conditions—the very definition of residents of nursing homes and assisted living facilities.
It is hard to know exactly when those older adults will begin getting the shots, but it likely will be over the next month or two.
That will mean the covid-19 nursing home nightmare may soon end. But the death toll has been staggering. And, worst of all, some of this tragedy could have been prevented.